The coagulopathy associated with COVID-19 has not been previously described in children and young adults. We reviewed the clinical and laboratory characteristics of children and young adults admitted for COVID-19 to an urban Children's Hospital in New York City, focusing on coagulation and venous thromboembolism.
Clinical and laboratory data were analyzed from 54 patients aged 2 months to 30 years treated by the Pediatric Hematology service at a single Children's Hospital between January 1 and May 31, 2020. Information was obtained from hospital records with IRB approval.
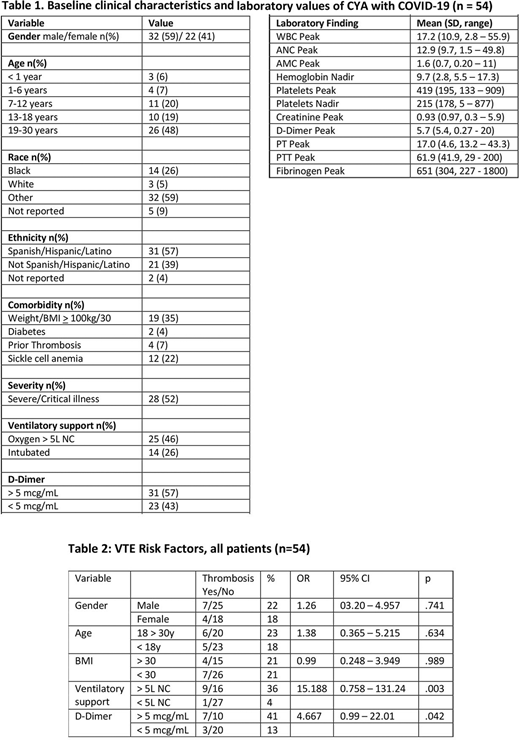
There was a moderate male predominance, with 32 (59%) males and 22 (41%) females. There were 28 (52%) patients younger than 18 years and 26 (48%) patients 18 - 30 years old. 26% of patients identified as Black, and 57% as Hispanic/Latino, similar to the community demographics in the Bronx in the 2019 census. Obesity was the most prevalent comorbid condition, with 19 (35%) patients having BMI of 30 or higher. There were also 12 (22%) patients with sickle cell anemia.
There were 28 (52%) patients in this cohort with severe and critical illness, as based on established criteria, and 25 (46%) patients required increased ventilatory support. This was defined by the need for > 5L nasal cannula, high-flow nasal cannula, non-rebreather, or intubation. 11 patients (20%) had documented venous thromboembolism (VTE). Four patients died of COVID-19 complications at ages 2 months, 11, 14 and 18 years old. The VTE rate was similar in those patients under 18 years of age (5 of 28, 18%) and those 18 - 30 years of age (6 of 26, 23%). Most (94%) patients had a D-Dimer > 0.5 (upper limit of normal) at admission and 57% developed peak D-Dimer > 5 ug/mL during their admission.
Elevated D-dimer > 5 was a risk factor for VTE with 3 of 23 (13%) and 7 of 17 (41%) patients developing VTE with D-dimer < 5 and > 5, respectively (OR 4.7, p=0.042). Patients requiring increased ventilatory support had a 36% rate of VTE as compared to 1 of 28 (4%) of those without (OR 15.2, p=0.003). Six of 24 patients on prophylactic anticoagulation developed VTE. One patient developed a pulmonary embolism 10 days post discharge from the hospital. No patients on anti-Xa-based low molecular weight heparin prophylaxis developed VTE. None of 12 patients with sickle cell anemia developed VTE, had peak D-Dimer > 5 ug/mL or required increased ventilatory support.
Hospitalized children and young adults with COVID-19 in our cohort developed a coagulopathy similar to that of older adults, characterized by elevated D-Dimer and high rate of VTE. This is in contrast to the published pediatric series out of China and Singapore that described mild illness and did not comment on VTE rates. Presence of elevated D-dimer or need for increased ventilatory support were significant risk factors for thrombosis. Patients with sickle cell anemia had a lower risk of VTE and less severe illness. Anti-Xa monitored thromboprophylaxis may aid in preventing or ameliorating the COVID-19 coagulopathy in children and young adults. Institutional anticoagulation guidelines were developed based on these observations.
Davila:Spire Learning: Speakers Bureau; ATHN: Other: Grant Funding. O'Brien:Bristol Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal